Key research challenges in validating immune system benefits



Sabina Lukovac is Division Manager Health at NIZO. In this column, with the help of other experts, she will be exploring some of the key issues and challenges facing the nutrition industry today.
In recent years, the nutrition industry has become increasingly interested in the immunity benefits of foods and supplements, with the corona crisis driving a particular spike in clinical trials over the past twelve months. And yet, the list of food components that have gained regulatory approval for immunity boosting claims is still limited to a handful of vitamins and minerals. To understand why and what can be done, I spoke to Anita Hartog, Senior Scientist Nutrition and Health at NIZO, who has over twenty years industrial experience studying the health and immunological impact of food.
Anita Hartog: Any health claim for a food or supplement needs verifiable evidence to support it, typically in the form of a clinical trial. For immune system benefits, this usually means a vaccination trial or infection challenge trial – both of with are very expensive to carry out. The results of the trial then need to be validated by the appropriate regulatory bodies such as the European Food Safety Authority (EFSA). And despite the spike in interest in this area, most trials sent to EFSA for validation are rejected because the quality of evidence just isn’t high enough. Hence, it is only the familiar vitamins B6, B9, B12, C and D plus iron that currently have approved immunity boosting claims.
AH: Pre-clinical studies on their own can’t deliver strong enough evidence for regulatory validation of a claim. But they do give you information on what to study and how best to do it. This in turn helps you design better clinical trials and improve the quality of the evidence they deliver.
There are various types of pre-clinical trial, each delivering different levels of evidence for a health effect; in vitro studies using carefully selected human cell lines, animal studies and ex vivo studies on actual people but without the challenge used in a clinical trial. Most nutraceuticals companies today want to avoid animal trials for ethical reasons. But recent developments in vitro models mean they can help to bridge that gap. In particular, these models are the ideal tool for screening food components to identify which one act on the immune system and for exploring their mechanism of action. And because the gut is such a key part in both our digestive and immune systems – around 70% of our immune cells are in our gut – in vitro models of the gut are the ideal place to start exploring potential immunity boosting claims for foods.

AH: In vitro models work by introducing the food or component under study to relevant human cells. Until recently, they looked at just one cell type. But increasingly, people are combining different types of cells into a single model to give a more complete picture of how a food component interacts with the human body. For example, to look at the immunity impact of a component, you could combine intestinal epithelial cells with examples of the gut microbiota and / or immune cells.
Taking this idea further, so-called organoid models are gaining ground. These combine all relevant cell types into a kind of miniaturized organ. For example, an intestinal organoid may include epithelial, immune and all the other cell types in the intestine plus a mucus layer to better which also impacts the action of a nutritional component. In a sense, organoid models can act as a simpler alternative to animal testing without the ethical issues of using animals and with the added benefit of using actual human cells.
Early organoids were typically three-dimensional – often spherical – which made it difficult to introduce test components to the site where they would normally contact intestinal cells. But there have been a number of recent successes in culturing 2D organoids, so that you have apical and basolateral sites available both for adding nutritional components and for sampling.
AH: The more complex the model, the more realistically it can mimic the environment inside our bodies. But complex models also take longer to deliver results. So simpler, high-throughput models are best used in early explorations when you are screening multiple or very novel components to narrow down promising candidates for further investigation. The more complex models are useful later for precise validation of previously identified components and their specific effects.
AH: Although only a handful of vitamins and minerals have approved immunity claims, there are many other food components that could potentially boost immune systems. And all of them could be explored using in vitro models. For example, there are a number of amino acids that are required for a properly functioning immune system, while certain oligosaccharides can inhibit pathogens from binding to cells in the intestinal wall.
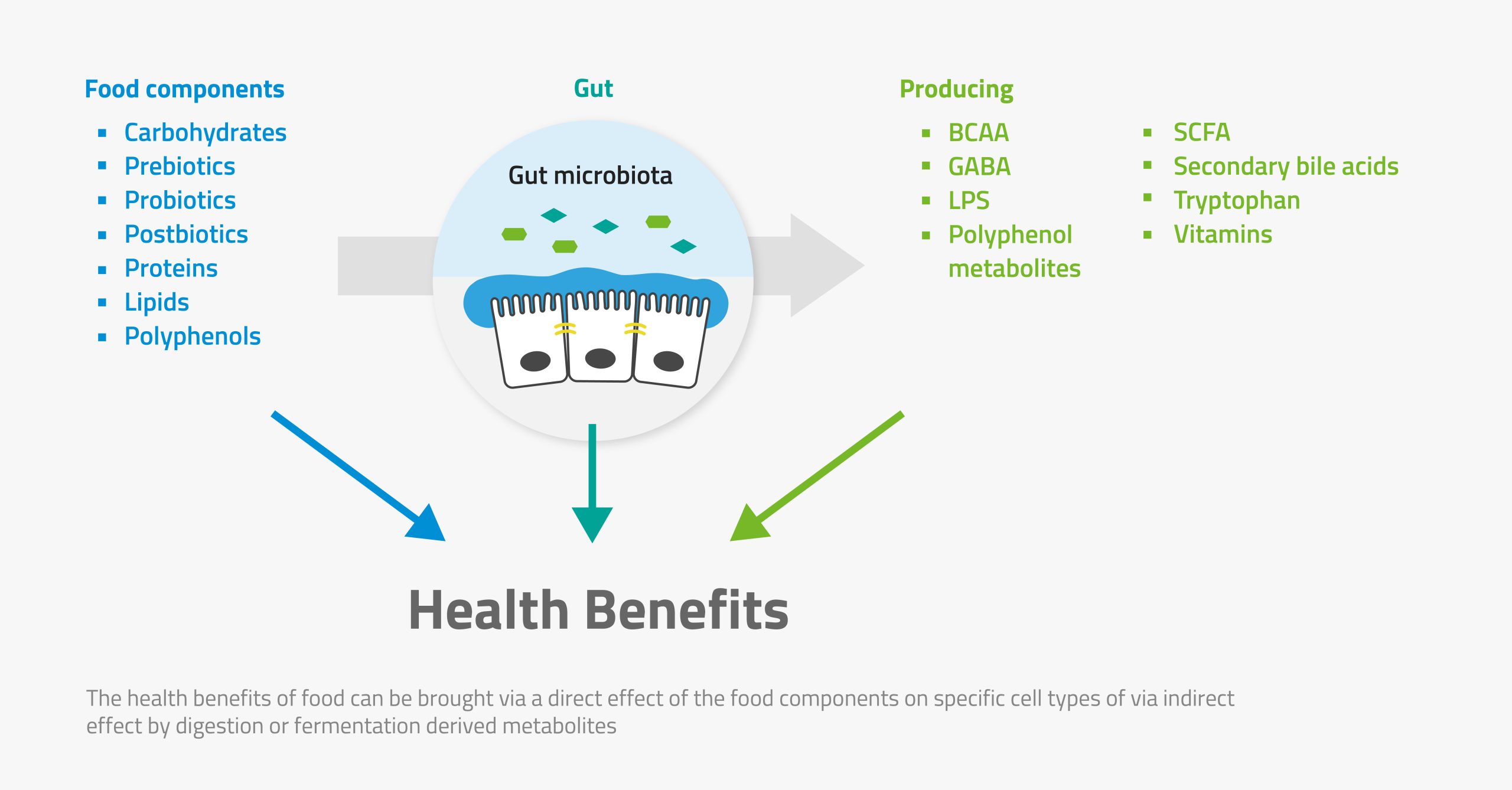
Interestingly, research by the International Probiotic Society last year showed that the gut microbiome plays a role in our immune response to diseases such as coronavirus. This suggests that probiotic microorganisms and prebiotics such as fibres could, in some cases, have an effect on immune systems. Indeed, there are clinical studies in the literature that report just such effects for probiotics and prebiotics, but they are not conclusive. In vitro models and pre-clinical trials certainly have role to play in improving the design of such studies.
AH: Food components can potentially impact the immune system in many ways, and all of them are accessible to testing through in vitro models. For example, you can look at the immune cells directly to see which particular components modulate activity such as pathogen engulfment. You can also look at the interaction between intestinal epithelial cell and immune systems, for example to see if a food component promotes or supresses the production of chemokines, signalling proteins that attract immune cells, in the presence of a pathogen. Or you can look at a whether a component can mediate a pathogen’s ability to disrupt the barrier that the gut wall represents.
AH: Food components can potentially impact the immune system in many ways, and all of them are accessible to testing through in vitro models. For example, you can look at the immune cells directly to see which particular components modulate activity such as pathogen engulfment. You can also look at the interaction between intestinal epithelial cell and immune systems, for example to see if a food component promotes or supresses the production of chemokines, signalling proteins that attract immune cells, in the presence of a pathogen. Or you can look at a whether a component can mediate a pathogen’s ability to disrupt the barrier that the gut wall represents.
In vitro models also allow you to explore the gut microbiome. You can look at what microbes are present in the gut, what they are doing and what they are producing. Then you can which specific prebiotics and probiotics modulate the microbiome’s functionality to make it more or less healthy.